Personal Medicine
On stumbling and stepping into the future of primary care
The Old Way
I often think about how annoying a certain kind patient must be to doctors these days. That patient who, having listened to the Huberman Lab podcast, or thumbed through the Peter Attia longevity book, comes into the annual physical full of annoying questions.
I am that patient.
The thing is, it hasn’t felt, for a long time, like anyone else is actually looking out for my health at all.
Every time I go in for my physical, there’s a new doctor. The last one “went into telemedicine,” another got shuffled out in a merger with an even bigger, less personal, goliath healthcare corp. Every appointment feels like starting from scratch.
I had my latest annual physical two weeks ago, with another primary care doc I’d never met. It didn’t go well.
I could tell when he walked in that he was pre-annoyed. His jaw was clenched, and he dropped heavily onto the stool across from me in a way that let me know he was not here for my shit. I became pre-annoyed back at him.
In the questionnaire I’d filled out in the waiting room, I’d asked about some additional bloodwork. I have a stacked deck in my family, and I’m holding a full house of cardiac and dementia risk.
When both my parents died of dementia within fourteen months of each other, I started reading up, wondering what I could do to reduce my risk of ending up like them.
I’ve run 23andme DNA reports, I’ve listened to the podcasts, and I’ve read the books.
These books and podcasts provide evidence-backed recommendations: simple blood tests that can help guide more personalized lifestyle changes, lowering our individual risks significantly. What a vast improvement this could be, compared to the same basic numbers and guidelines we’ve been working with for the past 30 years—medicine by flowcharts. Our parents’ medicine.
In that old school realm, some of my basic numbers are on the high side, but, according to the flowchart, it’s not time to do anything yet. It’s wait-and-see, fingers crossed.
I asked this irritated doctor about additional tests. An advanced lipid panel, for one. He asked why I wanted them, and I repeated the cardiac history. I told him my mom was only seventy-five when she died of dementia.
“Seventy-five’s not that young,” he said. Now we were both irritated. The doctor looked 60-ish. I wondered if he’d be okay spiraling into dementia fifteen years from now.
He tossed my questionnaire onto the table next to him and said. “I’m just not interested in any of this.”
“Or modern research, apparently,” I said quietly, but loud enough. That did it. He was out of there.
He left the room, leaving me unsure for a few minutes if the appointment was over. (It was.) I walked to my car, not super proud of either of us.
What I’d like as a patient is to feel looked after. I don’t want to feel like a bother for wondering how I can live healthier and longer. Isn’t that the whole point of an annual check-up?
This doctor I met with all too briefly is surely overbooked, underpaid, and under-resourced. That new healthcare goliath certainly isn’t looking after him. He’s just doing what he can to get through his shift without one more patient bogging him down with annoying questions.
He’s stuck, as most of us are, in reactive medicine. More often than not, that means only working with the patient–their cardiac issues, cancer, dementia–once there’s already a diagnosis. I watched this happen with my mom. It’s like calling in the fire department after the house is already engulfed in flames.
I want better smoke detectors.
A New Hope
Fortunately, there’s a new wave of medicine coming – what Peter Attia calls Medicine 3.0. This week, my second physical felt part of that new, promising future.
Bad news up front: it’s expensive, and of course, nascent. Availability is limited. Still, what I experienced felt like an absolute revelation.
I started by getting my own blood work, and joining a service called Forward, which purports to be “the future of personalized healthcare.” (I have zero affiliation with them, other than my membership.)
Forward is quick to caution: this should be in addition to having a primary care doctor, a layer on top, not a replacement.
I booked an appointment easily using their app, and arrived at the Forward office in NYC to find… nobody.
The waiting room was stunning and hypermodern, flat screens on multiple walls. There was soothing electronic music playing. One screen directed me to sign in, then directed me onto a 7-foot-tall scanner, where I stood on a scale, peered into a sensor, and inserted my fingers into capsules.
This all felt dystopian, like self-checkout for the human body. Luckily, an actual human–an ultra-friendly tech–popped in a few moments later.
The experience from then on was the perfect blend of humans + technology. My doctor was a warm, compassionate, ultra-knowledgeable primary care physician. We met in a patient exam room with a beautiful screen-wall that spun up graphics, outlining each step of our conversation as we spoke.
Diagrams popped up, as well as my family history, genetic profile, blood work results—graphic modules that she could tap and expand. It was like CNN on election night, only the touch display worked.
“I want to help my patients to be in charge of their own health,” she told me. “Only you can tell me how you actually feel, what you’re doing and not doing—and most importantly, what makes sense for how you want to live. Data helps inform us, and then I help you come up with your individual plan, which we modify as we go.”
This is it, I thought.
My plan includes learning which specific foods cause my blood sugar to spike, with a few weeks on a continuous glucose monitor. This is important, as blood sugar spikes are suspected to contribute to dementia.
I’m also now on a low-dose statin, I’m adding even more high-intensity exercise to my week, and I’m seeing which dietary changes might move my cholesterol and other biomarkers into a more favorable range. It’s all experimentation–leveraging data—to find out what works in my particular case.
So this new paradigm is arriving, but it’s still cost-prohibitive. It takes commitment and effort on the patient’s part. Huberman podcast episodes and the Attia book are long. There’s the very real risk of feeling like you’re joylessly tracking every step and bite. Optimizing yourself into oblivion. Each person has to find the balance that works for them.
Like all new frontiers, Medicine 3.0 is still rocky and under-populated. But I’ve seen where we’re heading, and it gives me hope.
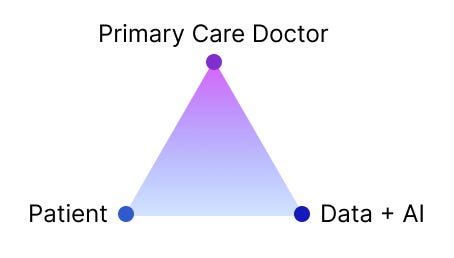
Patients will be better informed, and empowered to know what they’re doing and why. They’ll provide ongoing self-reports on general well-being and symptoms.
Data & AI will bring lower-effort tracking over time, allow highly customized programs and plans, flagging anything notable, and surfacing new research and evidence-backed treatments for the doctor to review.
Primary care doctors will coordinate this 3-part team, working with the patient and AI to guide individualized care, with less time spent on documentation and research, and more time for patient care.
We’ll always want that human doctor, no matter how good AI gets. In that hyper-digital Forward waiting room, I had the sinking feeling that it was just me and the robots. I felt the exact same bleakness, though, in that unfortunate first physical, with the doctor who saw me as another quick task to be initialed and marked complete.
In the meantime, while we await the future, I’m still looking for a good GP. Now that I have a few more answers, I’ll be a little less anxious in my next appointment, and hopefully a little more understanding of the primary care doc’s plight, too. I want a better, more human experience for both of us, where nobody feels pre-annoyed, and both of us feel understood, and looked after.
If you enjoyed this post, please hit the heart ❤️ and share it with a friend. I’d also love to hear your thoughts in the comments. Either way, I appreciate your being here.
Further reading: I highly recommend Longevity Minded by Jack Dixon. Paying subscribers can access an annotated summary of Peter Attia’s longevity book, Outlive (67 pages instead of 500) which is well worth the price of subscription alone.
Massive thanks to Miche Priest of Started on Tolkien for the early read and invaluable feedback. 🙏








"What I’d like as a patient is to FEEL looked after."
It's amazing how little this would take and at the same time how low this bar is. Instead of feeling threatened by the availability of information, there's an opportunity to embrace it and use technology to improve health outcomes. Leveraging technology enables human doctors to be more...human. Unfortunately the business of medicine ends up taxing doctors instead of capitalizing on the opportunity to provide compassionate care.
This turned out great Rob.
Excellent essay Rob. Your first appointment encounter perfectly captures that inner feeling of hopelessness when it comes to healthcare. Good luck with your health journey. Curious about the new model you describe.